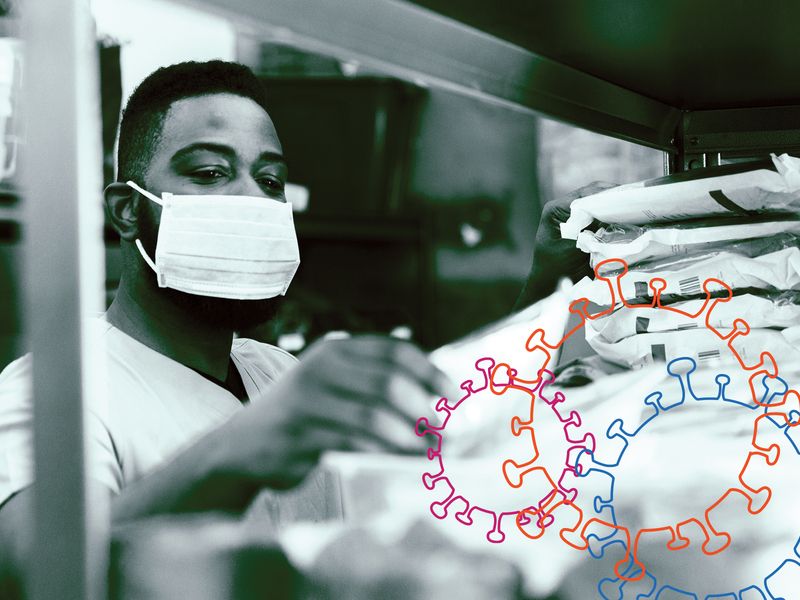
A shortage in the Strategic National Stockpile even before the pandemic and the failed efforts of multiple agencies to coordinate access to personal protective equipment endangered the lives of healthcare workers and weakened the efficacy of American hospitals, lawmakers and experts testifying before a Senate committee Wednesday said.
“Despite years of warning about the dangers of our nations over reliance on foreign sources and manufacturers for medical supplies our nation was still unprepared to treat a significant number of covid patients, stop the spread of the virus, and save lives,” said Senator Gary Peters (D-MI) in his opening remarks.
Over 580,000 civilians and 4,000 healthcare workers died during the pandemic.
Shereef Elnahal, President and CEO of Newark New Jersey University Hospital, said far more would have perished had the CARES Act not provided funds for hospitals to purchase more supplies.
“We have found ourselves at risk of running out of supplies that we have never seen depleted before, including PPE for staff and ventilators for patients that needed it,” said Elnahal. “We were days away from patients being without key medications, such as sedatives for those on a ventilator.”
“American exceptionalism became American hubris,” said Dr. Robert Handfield, Professor at North Carolina State University. “No one knew where products were coming from, whether they were being sent, and who was receiving them. The response was too little too late.”
There is no current federal policy to distribute materials in an emergency based on need, meaning some were randomly allocated. In other cases SNS inventory expired before getting to providers.
Handfield recommended the government enter into contractual incentives with agencies like the Veterans Affairs Department to “turn around inventory,” and investments in “material visibility technology” to forecast where supplies should be allocated. The goal would be to protect the supply chain against an overreliance on foreign products and a lack of diversity in manufacturing supplies. Experts said the stockpile was unprepared to meet these shortcomings in the supply chain as the demand for medical supplies grew during the pandemic.
“The stockpile was made to respond to discrete emergencies, often at the expense of pandemic preparedness,” said Senator Rob Portman (R-OH). According to the committee, the stockpile had not been replenished following the breakout of H1N1 influenza virus in 2009.
Meanwhile, Elnahal said value-based payment reform could help hospitals’ financial solvency and supplies.
When hospitals were forced to shut down, they lost revenue and the liquidity to replenish resources.
Independent hospitals like Elnahal’s ended up bidding for supplies. Many of those suppliers were outside the medical community’s supply chain, resulting in resources that were often fraudulent or ineffective.

 health
health